Masood Mansour, MD
by Erin Walsh

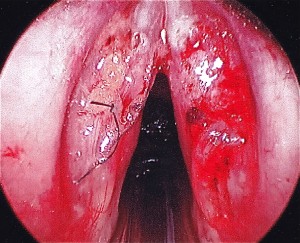
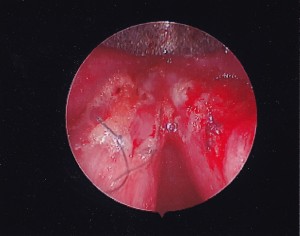
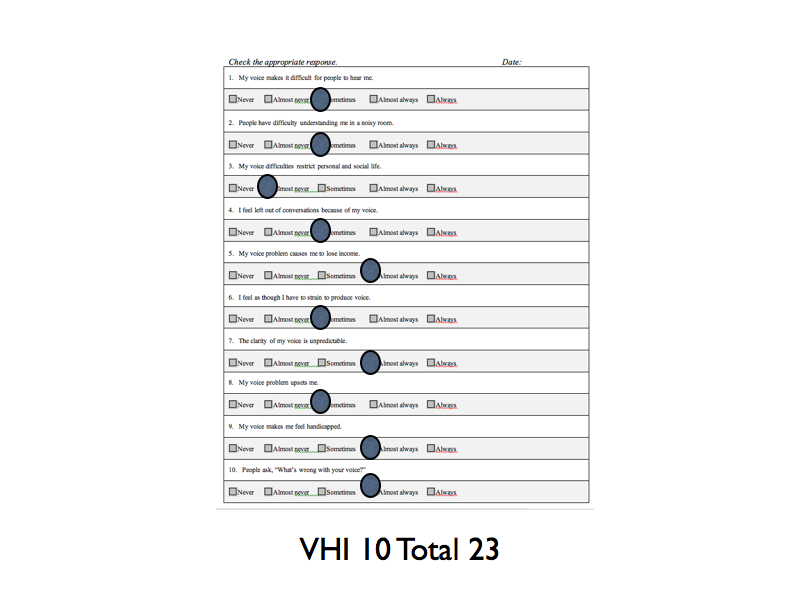
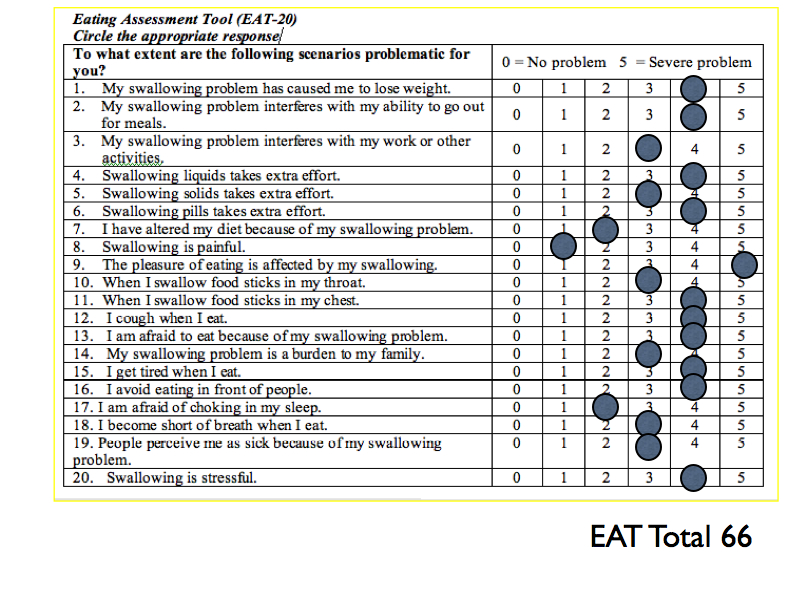
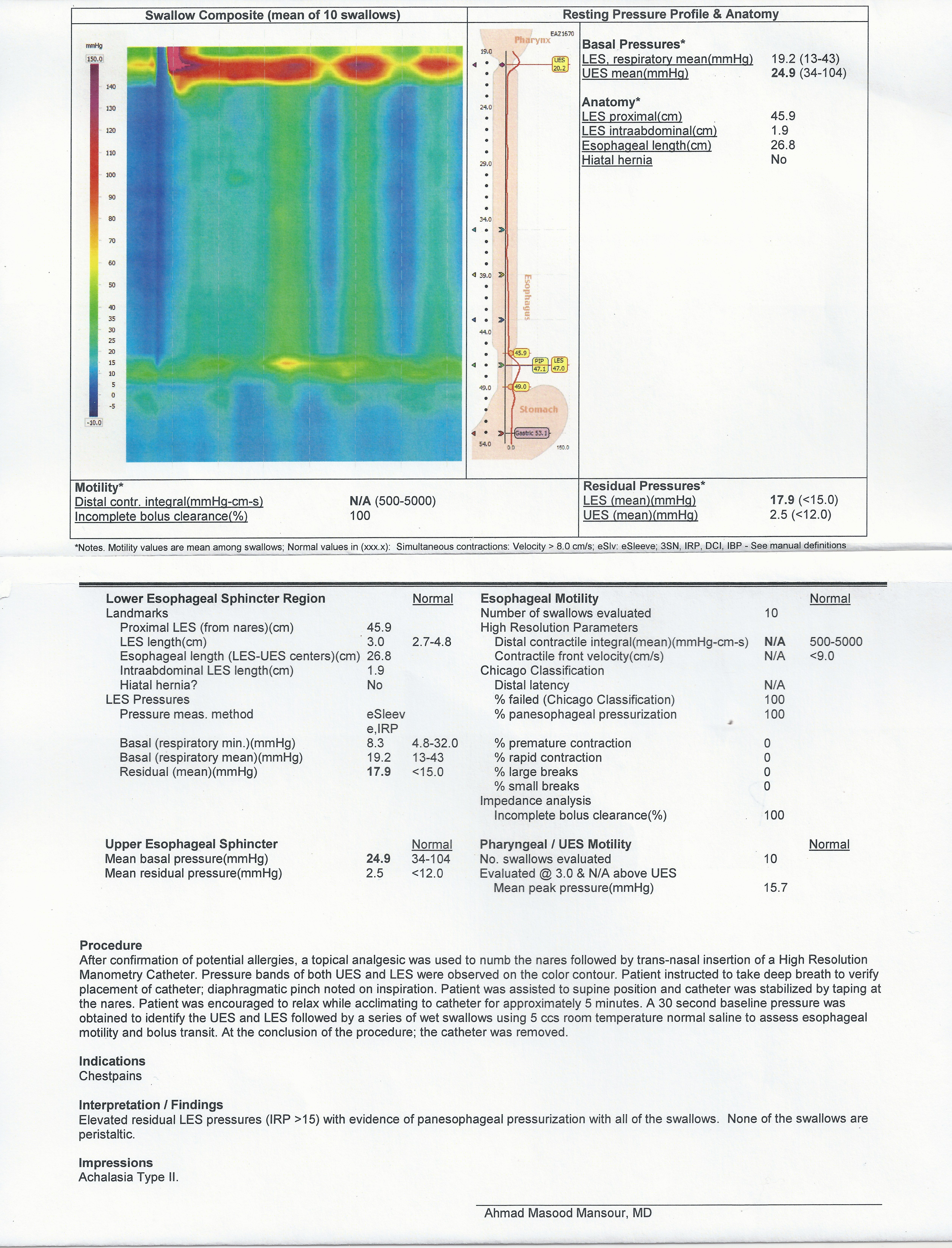
Case: Healthy 19yo male with 10 month history of chest pain, nausea, vomiting and dysphagia. He struggles to consume both liquids and solids, resulting in a 30lb weight loss. Trial of PPI and Reglan did not improve his symptoms. EGD 4 weeks ago revealed mild gastritis. Biopsies were normal. Esophagram demonstrated poor lower esophageal sphincter relaxation.
PMH: Generally unremarkable. Ear infections.
Social: Sophmore in college.
High Resolution Manometry:
Treatment: Discussed with patient and his family variety of options to manage his condition. 1) Botox – not recommended due to age and need for repeat injections 2) Pneumatic dilation – norms for good response to this therapy are on females older than 45. There is risk of perforation and it is likely repeat dilations will be required. 3) Myotomy with partial fundoplication – long-term solution to his condition. This was the recommended course of therapy. Risk of post-operative reflux was discussed. After speaking with the laparoscopic surgeon, the family ultimately decided on option #3.
Surgery: Uncomplicated laparoscopic esophageal Heller myotomy with Dor fundoplication. Initiated a soft diet on post-op day 1. Mild abdominal epigastic tenderness and discomfort so on post-op day 2 underwent esophagram to assure no leak. The study revealed no obstruction and no Gastrografin leak. He was discharged home on post-op day 2.
Outcome: 11 days after surgery feels well, no fatigue or pain. Nausea and vomiting resolved. He is able to eat and drink anything. Although he has not gained weight, he exhibits an appropriate body mass index. Prior to developing achalasia, he was approximately 20lbs overweight.
 Presenter:
Presenter: