Voice problems can develop at any age. They do not always result from trauma such as yelling, coughing or reflux. Sometimes changes in voice are due to medication side effects, inadvertent nerve damage from surgery, viral nerve paralysis, HPV, cancer or neurological conditions. Below are examples of a variety of voice conditions and a brief description of how they typically develop. Treatment for voice disorders should begin with an ENT doctor, preferably with specialty in laryngology. Be certain to inquire whether your doctor uses a strobe light when they perform endoscopy to look at your vocal cords. This allows for clear and accurate depiction of the vocal cord tissue and assessment of vibratory integrity. An endoscopy without stroboscopy prohibits assessment of this movement, which may be essential in determining the source of hoarseness. If the condition you are experiencing is related to breathing difficulty, as in vocal cord disorder (VCD), the managing physician may be a pulmonologist or allergist. The ENT may decide to pursue surgery, therapy with a speech pathologist who specializes in voice disorders, or both.
Muscle Tension Dysphonia
MTD means excessive throat compression is occurring during speech or singing. It typically manifests as a secondary response to an underlying voice conditions such as vocal cord weakness (paresis or paralysis), growths on vocal cords, reactive to reflux exposure in throat, general hypersensitivity from medication, allergies, post-nasal drip or environmental irritants. It is important to explore all potential causes before trying voice therapy to change speaking patterns because the condition may reverse itself without direct intervention. There are rarer cases where MTD expresses itself without organic triggers seen in the larynx. This may occur with psychological distress and often requires direct intervention with a voice therapist to train relaxed speaking patterns. Concurrent counseling or psychiatric services may be warranted.
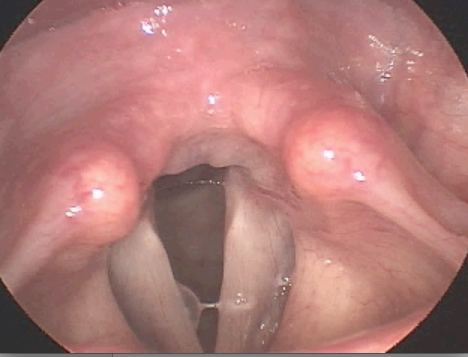
Vocal Nodules
Vocal nodules are symmetrical calluses that develop on the free edge of the vocal cords. They form from chronic traumatic vocal cord closure such as loud talking, yelling, unhealthy singing, coughing and throat clearing. These conditions may result from more indirect causes such as reflux, stress, post-nasal drip, dehydration or allergies. The calluses are similar as to what a guitarist would develop on the fingers he used to hold the strings on his fret board. As long as there is no additional pathology identified such as a polyp or cyst, the callusing will resolve once the behavior causing it stops. This occurs in voice therapy where a specialized speech pathologist will help modify speaking and singing styles to reduce excessive compression of the vocal cords.
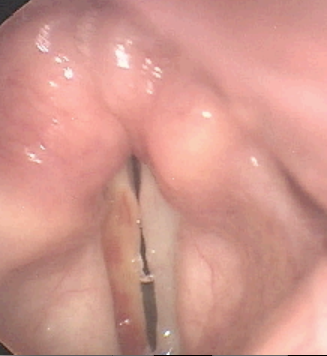
Vocal Cyst(s)
Cysts usually develop on one vocal cord and may cause callusing where it strikes the contralateral side. They are not necessarily caused by overuse; however, can be worsened in a person who uses their voice excessively. Formation of a cyst is typically the result of a blocked glandular duct or abnormality of a mucous membrane. They are differentiated from a polyp in that the lesion is typically dense and inflexible. The voice quality of a cyst is generally characterized by persistent hoarse/harsh quality, whereas a polyp may result in intermittent normal quality due to the flexibility of the lesion. Treatment involves surgery with an ENT doctor. Your doctor may refer you for peri-operative vocal therapy to reduce compensatory muscle tension speaking patterns.
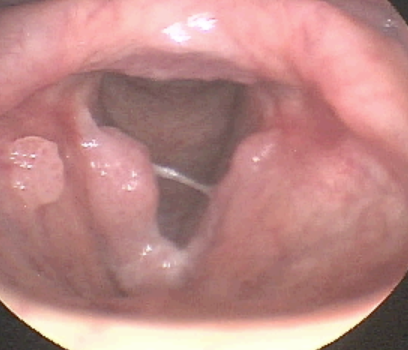
Vocal Polyp(s)
Polyps are fluid filled sacs that form on the striking surface of the vocal cords. In contrast with vocal nodules, it is possible for a polyp to develop on one or both vocal cords from a single traumatic event. They also occur from chronic overuse. Some believe polyps are resolutions of prior hemorrhages, whereas an individual speaks through the bleeding and an organized fluid filled sac develops. Depending on the stage of the polyp and vascular structure of the vocal cord, the polyp may be acutely hemorrhagic. The resulting vocal quality of a polyp will often differ from a cyst and/or nodules. Due to the hypermobility of the fluid, sometimes the striking zone of the vocal cords is clear and the voice will sound normal. Management of medium to large polyps almost always involves surgery with peri-operative vocal therapy to reduce traumatic speaking/singing patterns. In some cases, the vocal cords are excessively swollen and may appear to be nodules. As an individual begins voice therapy and swelling reduces, the nodules may evolve and reveal a polyp or cyst.
Vocal Fold Hemorrhaging
Hemorrhaging is an acute vocal cord condition requiring absolute vocal rest to heal without potential of causing permanent damage to the tissues. It may happen from yelling, coughing, sneezing, laughing or other circumstances that induce forceful traumatic vocal cord closure. Dehydration and blood thinning medications can cause predisposition to hemorrhaging. Vascular structure of each person's individual vocal cords also determines risk of hemorrhage. If a singer who prefers belting style has large blood vessels along the striking surface of the vocal cords, they are at particular risk. ENT doctors will sometimes remove the blood vessels on the vocal cords to prevent hemorrhaging, especially if there is chronic inflammation or prior nodules/polyps/cysts.
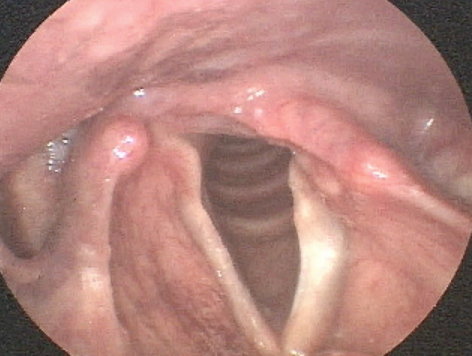
Laryngeal Papilloma
Vocal cord papilloma are irregular growths resulting from infection of human papilloma virus (HPV). They can cause severe hoarseness and even breathing difficulty depending where they grow in the throat and airway. Laryngeal expression of HPV occurs in only a small number of people who carry the virus. It may recur many times or lay dormant for long periods of time. Treatment of vocal cord papilloma requires surgery. This typically is achieved with a laser and may need to be performed on multiple occasions. There is a role for voice therapy in papilloma cases, as the repeat growths and surgeries may cause compensatory muscle tension or chronic scarring/stiffness of the vocal cords.
Vocal Fold Paralysis
Vocal cord paralysis or paresis (partial paralysis/weakness) occurs when there is damage to the laryngeal nerve(s). This can develop for a variety of reasons including viral infections, neck surgeries (cervical spinal fusions), thyroid removal, intubation and trauma anywhere on the neck. Left vocal cord paralysis is more common than right vocal cord paralysis because the nerve on the left side loops below the heart. Some patients who undergo heart surgeries sustain vocal cord paralysis due to damage of this nerve. Prognosis for vocal cord paralyses varies. If it is believed the injury is due to viral illness or bruising/stretching with a surgery and the voice is beginning to return, it may completely resolve without intervention. Temporary vocal cord injection can be performed by an ENT surgeon to alleviate hoarseness and swallowing difficulty. If there is a known cut to the nerve due to surgery or injury and the voice has remained persistent breathy without any change, it is likely the patient will require permanent augmentation of this vocal cord where the surgeon pushes the vocal cord to the middle so it can meet the other side, creating improved speaking quality.
Irritable Larynx Syndrome: Paradoxical Vocal Fold Movement, Vocal Cord Dysfunction, Laryngospasm, Chronic Cough, Chronic Throat Clearing, Muscle Tension Dysphonia
Irritable Larynx Syndrome may manifest with any of the aforementioned conditions. It is the result of nerve hypersensitivity. The 10th Cranial Nerve, called the Vagus Nerve, branches off to the throat, esophagus and stomach, among other places. Sometimes this nerve can become hypersensitive and cause chronic irritation. The hypersensitivity may be the result of a virus, surgical injury, response to a medication, reflux, post-nasal drip, allergies or stress. Once factors such as reflux, allergy and medication management have occurred, there is a role for vocal therapy where behavioral suppression of coughing, throat clearing and laryngeal tension occur. Paradoxical Vocal Fold Movement (PVFM), also called Vocal Cord Dysfunction (VCD) may manifest only as breathing difficulty and often is confused with asthma. Asthma involves difficult with exhalation, whereas PVFM involves difficulty with inhalation and may be accompanied by a gasping noise called stridor. It is possible to suffer from both conditions. If asthma inhalers are ineffective, the breathing difficulty comes on and resolves rapidly (within minutes), it is suspicious of PVFM. Treatment for this condition is accomplished with a speech pathologist who will provided tailored approach for disengagement of laryngeal muscles to allow for comfortable breathing.
Neurological Disorders: Spasmodic Dysphonia, Tremor
There are three variations of spasmodic dysphonia, which involves involuntary spasms outward and/or inward of the vocal cords. The types include adductor spasmodic dysphonia (ADSD), abductor spasmodic dysphonia (ABSD) or mixed spasmodic dysphonia. This unfortunate diagnosis can severely impede the ability to talk. Voice therapy may be useful in providing strategies to speak around the spasms, but will not cure the condition. Recurrent Botox injection is the most common form of management for spasmodic dysphonia. Some patients eventually undergo nerve surgery in attempt to stop the spasms. Tremor is another condition that can be highly disruptive to vocal clarity. It is more difficult to manage. Vocal therapy typically addresses modifications to speaking style in attempt to hide the tremor such as pitch, speaking rate and inflection. Medical management for tremor may involve trial of medications or Botox. The tremor may be local to the throat muscles or also present in other parts of the body.