Presenter: Priya Krishna, MD, MS, FACS
Presenter: Priya Krishna, MD, MS, FACS
Director of Voice & Swallowing Center at Loma Linda Medical Center
Dr. Krishna is board certified in otolaryngology and completed a prestigious two year fellowship in Laryngology and Care of the Professional Voice at the University of Pittsburgh Medical Center under Clark Rosen, M.D., F.A.C.S. Prior to this she completed a residency in Otolaryngology-Head and Neck Surgery at the Southern Illinois University School of Medicine. Dr. Krishna served as faculty in the Department of Otolaryngology at the University of Pittsburgh Medical Center from 2006 to 2011 while concurrently completing a Master of Science degree in Clinical Research. Dr. Krishna specializes in surgical and medical care of voice, airway and swallowing disorders including phonomicrosurgery of benign and early malignant lesions of the vocal folds, office laser based procedures for laryngeal pathology, endoscopic treatment of airway stenosis and neurological disorders of the larynx. She has a special research interest in treatment of vocal fold scarring and related wound healing disorders of the larynx and has been funded extramurally (including federal) for her work in the past.
CASE: 23 y/o female swim instructor presents with complaints of trouble projecting voice, vocal fatigue with use and progression over 6 months. Voice rest is helpful.
PMH: systemic lupus erythematosus, rheumatoid arthritis, thrombotic thrombocytopenic purpura, antiphospholipid antibody positive, hx of pulmonary embolism
ROS: unremarkable except for HPI
ALLERGIES: humira, rituximab
MEDS: abatacept, calcium carbonate, ferrous sulfate, plaquenil, levonorgestrel, prednisone, warfarin
SOCIAL: non smoker, social ETOH, swim instructor with high voice demands.
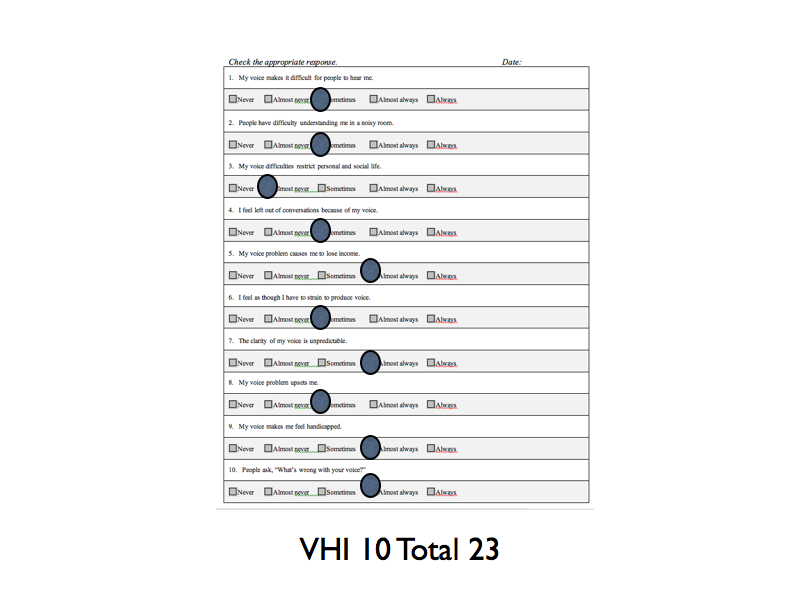
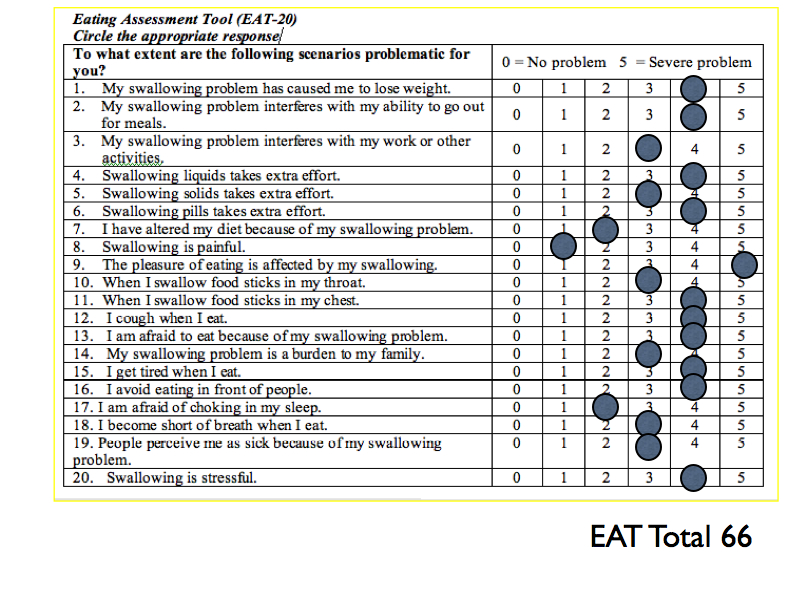
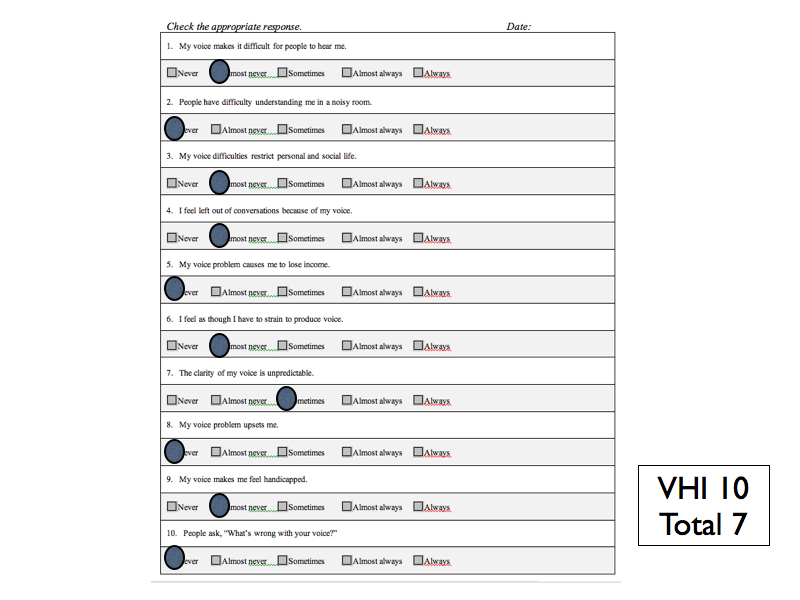
SELF RATINGS: Voice Handicap Index-10 = 33 Reflux Symptom Index = 9
PHYSICAL EXAM: hoarse voice, scant intranasal mucus, otherwise unremarkable
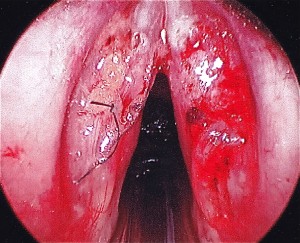
STROBE: Bilateral mid membranous vocal fold lesions with decreased mucosal wave and amplitude. Hourglass glottal closure. Left VF lesion larger in size than right vocal fold lesion. Bilateral vocal fold erythema, edema and moderate varices. Normal mobility of bilateral vocal folds.
TX RECOMMENDED: Microflap excision of bilateral vocal folds lesions and bilateral fat implantation followed by voice therapy. Second option was injection of vocal folds with steroids, which may take multiple treatments but can also be effective. Pt desired a one time surgical treatment.
SURGERY: Pt underwent microsuspension direct laryngoscopy with microflap excision of bilateral vocal fold lesions, abdominal fat harvest with bilateral fat implantation.
 |
 |
 |
OUTCOME: Pathology c/w vocal fold cysts with elements of rheumatoid nodules (multinucleated giant cells).
1st POST-OP SELF-RATINGS: Voice Handicap Index -10 = 38 Reflux Symptom Index = 7
STROBE: Exam indicates healing vocal folds with reaction to fat and suture but good augmentation both vocal folds; lack of mucosal wave bilateral and “splinting” posture of larynx.
2nd POST-OP SELF-RATINGS: Voice Handicap Index -10 = 29 Reflux Symptom Index =not completed
STROBE: Decreased edema and erythema of bilateral vocal folds, decreased mucosal wave. Much improved from previous postoperative exam.
FOLLOW-UP: Continues to improve with time and voice therapy.