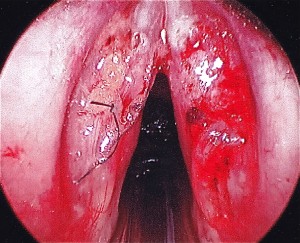
Recently I had the pleasure of working with a brilliant woman enjoying a successful singing career as an avante-garde performer with trademark vocal acrobatics and multiphonics. Through experimentation, she taught herself to produce different tones simultaneously. Once you listen to her unusual vocal style, you may assume misuse generated her referral. Not so. And I am certainly in no place to advise her to discontinue a performance style she is passionate about and has never left a shred of vocal pathology. On the contrary, I was grateful to learn from her skill to share with other vocalists how to safely produce tones some may classify as screaming. I have seen these produced in unhealthy manners with devastating after effects, namely hemorrhaging and vocal cord scarring. A singing sample and her laryngeal videostroboscopy are provided below. There two aspects of her endoscopy you may find intriguing. First, her vocal cords are in pristine condition. They are pearly white and exhibit healthy edges. The edges of the vocal cords are generally where a pathology would arise from overuse due to repeated forceful closure. Secondly, when I ask her to reproduce simultaneous pitches, you will notice she elicits two vibrations in different quadrants of the vocal cords. Generally, we see one vibratory collision involving the entire true vocal cord. I was grateful for this opportunity to work with such an energetic performer and explore the technical skill of her vocal style. -Erin Walsh
Priya Krishna, MD, MS, FACS

Director of Voice & Swallowing Center at Loma Linda Medical Center
Dr. Krishna is board certified in otolaryngology and completed a prestigious two year fellowship in Laryngology and Care of the Professional Voice at the University of Pittsburgh Medical Center under Clark Rosen, M.D., F.A.C.S. Prior to this she completed a residency in Otolaryngology-Head and Neck Surgery at the Southern Illinois University School of Medicine. Dr. Krishna served as faculty in the Department of Otolaryngology at the University of Pittsburgh Medical Center from 2006 to 2011 while concurrently completing a Master of Science degree in Clinical Research. Dr. Krishna specializes in surgical and medical care of voice, airway and swallowing disorders including phonomicrosurgery of benign and early malignant lesions of the vocal folds, office laser based procedures for laryngeal pathology, endoscopic treatment of airway stenosis and neurological disorders of the larynx. She has a special research interest in treatment of vocal fold scarring and related wound healing disorders of the larynx and has been funded extramurally (including federal) for her work in the past.
CASE: 23 y/o female swim instructor presents with complaints of trouble projecting voice, vocal fatigue with use and progression over 6 months. Voice rest is helpful.
PMH: systemic lupus erythematosus, rheumatoid arthritis, thrombotic thrombocytopenic purpura, antiphospholipid antibody positive, hx of pulmonary embolism
ROS: unremarkable except for HPI
ALLERGIES: humira, rituximab
MEDS: abatacept, calcium carbonate, ferrous sulfate, plaquenil, levonorgestrel, prednisone, warfarin
SOCIAL: non smoker, social ETOH, swim instructor with high voice demands.
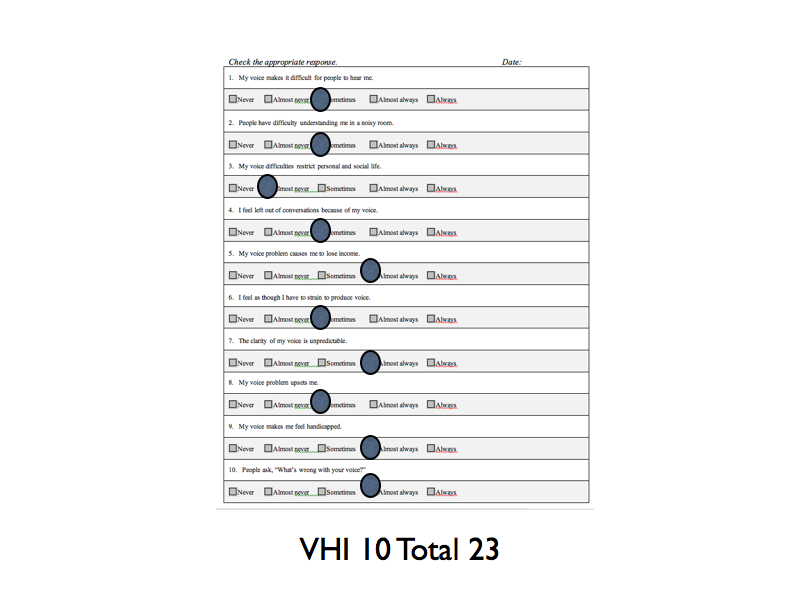
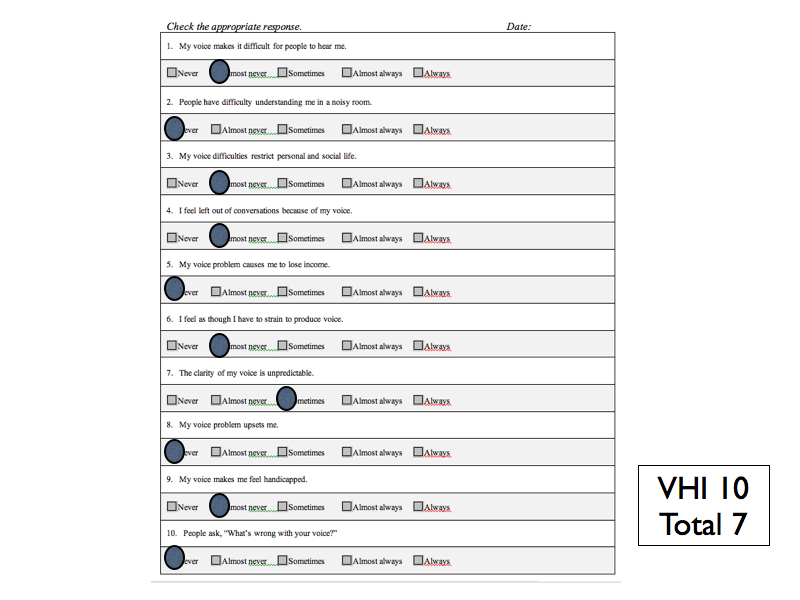
SELF RATINGS: Voice Handicap Index-10 = 33 Reflux Symptom Index = 9
PHYSICAL EXAM: hoarse voice, scant intranasal mucus, otherwise unremarkable
STROBE: Bilateral mid membranous vocal fold lesions with decreased mucosal wave and amplitude. Hourglass glottal closure. Left VF lesion larger in size than right vocal fold lesion. Bilateral vocal fold erythema, edema and moderate varices. Normal mobility of bilateral vocal folds.
TX RECOMMENDED: Microflap excision of bilateral vocal folds lesions and bilateral fat implantation followed by voice therapy. Second option was injection of vocal folds with steroids, which may take multiple treatments but can also be effective. Pt desired a one time surgical treatment.
SURGERY: Pt underwent microsuspension direct laryngoscopy with microflap excision of bilateral vocal fold lesions, abdominal fat harvest with bilateral fat implantation.
 |
 |
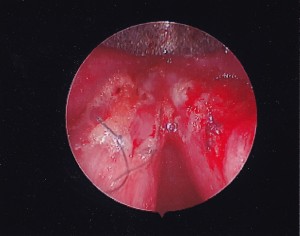 |
OUTCOME: Pathology c/w vocal fold cysts with elements of rheumatoid nodules (multinucleated giant cells).
1st POST-OP SELF-RATINGS: Voice Handicap Index -10 = 38 Reflux Symptom Index = 7
STROBE: Exam indicates healing vocal folds with reaction to fat and suture but good augmentation both vocal folds; lack of mucosal wave bilateral and “splinting” posture of larynx.
2nd POST-OP SELF-RATINGS: Voice Handicap Index -10 = 29 Reflux Symptom Index =not completed
STROBE: Decreased edema and erythema of bilateral vocal folds, decreased mucosal wave. Much improved from previous postoperative exam.
FOLLOW-UP: Continues to improve with time and voice therapy.
Dysphagia Support Groups: Personal lessons learned
I have had the pleasure of working with individuals with dysphagia for almost 17 years. This experience has provided a plethora of learning opportunities that have transcended well beyond the clinical realm.
We as clinicians often focus all of our energies managing the physiologic effects of the disorder on our patients. We frequently lose sight of the emotional toll that is also involved. This is what prompted my interest in starting a dysphagia support group. The decision was sparked by an overt influx of patients with severe-profound dysphagia. Each of these patients relayed a story that reflected similar themes. Specifically, they spoke of the impact of dysphagia including altered quality of life, social isolation and depression. It became clear that as a clinician, I had a responsibility to provide a safe forum to share these thoughts and emotions with one another.
In preparation for my group, I developed a rigorous agenda that included multiple educational topics. I created nametags and fliers and started to pass them out to all of my patients. Unfortunately, I have limited space for the meeting, so I had to limit our initial session to 5 people including patients’ caregivers. I enthusiastically presented my plan to the group that included a long list of learning objectives. Upon completion of my spiel, I took note of the uncertainty of the group. This sparked learning opportunity #1: “Ask your group about their personal objectives”. Once I asked that basic question, the proverbial floodgates opened and I received extraordinary information. Learning opportunity #2: “Give the group time to develop a strong and safe relationship with one another”. Developing this intimacy is what allows the group to flourish. Patients need to speak honestly and candidly with each other. This is when you will see the true benefits of the forum as patients/caregivers graciously share their thoughts and emotions. Learning opportunity #3: “Keep the group small and choose the group wisely”. Initially, I had a vision of filling a small auditorium with a diverse grouping of patients with dysphagia: WRONG. In my opinion, the ideal group should include approx 5 patients with their family/caregiver. The small forum will allow for maximum participation and comfort. Similarly, patients should be somewhat homogenous regarding the severity of their disorder. Placing patients with mild dysphagia with others who are feeding tube dependent may inspire negative feelings for participants. Learning opportunity #4: “Our job is to facilitate and allow for honest, albeit uncomfortable discussion”. It’s easy to assume that support groups should resemble a “Kum Bah Yah,” that they should be soft and light and make everyone feel great. Unfortunately, the nature of dysphagia creates sad, uncomfortable and sometimes confrontational dialogue between participants. The role of the facilitator is to allow for respectful interplay with some redirection if the discussion becomes hurtful. I have seen wonderful results emerge from difficult interactions. Last but not least, learning opportunity #5: “If your boss says ‘no’ to your idea to host a group, keep fighting until he/she says ‘yes’”. I have found that there are creative ways to fund these groups. Our organization allows for billing hours into a community benefit cost center. This gives me a small amount of time to prepare for and host our meetings.
My sincere hope is that more and more clinicians will embark on this journey. Hosting groups is gut wrenching, however, it complements everything and we stand for. I pride myself on spending countless hours on advancing my education and clinical experience through courses and self-study. Ironically, I feel as if I have learned more about dysphagia and the patients’ I treat through this amazing group venue.
Best regards and Good Luck!
Liza Blumenfeld
Newsletter
Medicare Therapy Cap:
What patients and clinical service providers need to know.
Background: The “Balanced Budget Act of 1997” imposed a $1,500 cap on outpatient therapy services. Section 4541 (c) and (d) of the act increased the financial limitation to no more than $1500 of the incurred expenses in a calendar year, and applied it to outpatient therapy services furnished in skilled nursing facilities, physician’s offices, home health agencies (Part B), skilled nursing facilities (Part B), in addition to private practice offices. This cap did not apply to hospital-based outpatient programs. The effective date of this $1,500 cap was January 1, 1999. A myriad of legal actions were successful in delaying implementation of the cap, until it cleared all barriers and went into effect on January 1st, 2006. Later that year, congress generated legislation that created an exception process, thereby allowing continued care for specified patients that have exceeded the cap.
In early 2012, President Obama signed into law The Middle Class Tax Relief and Job Creation Act (H.R. 3630). This legislation mandated that Hospital-based outpatient would be subject to the therapy cap process beginning in October, 2012.
Unless legislation is passed, Beginning on January 1st, 2013, the exceptions process will no longer be in effect and all outpatient therapy settings, excluding hospital based outpatient programs, will be forced to strictly adhere to the therapy cap provisions.
Understanding the current process:
The current therapy cap amount is $1800 for Speech Therapy and Physical Therapy combined. It is unclear as to why two disciplines share the cap amount. Through the exceptions process, patients may receive additional services in excess of the cap, if clinicians identify continued need for skilled therapy. In 2012, there are two exception processes: an automatic exception and a manual medical review process. The automatic exception to the therapy cap can be utilized to extend patients’ services from $1880 to $3700. No prior authorization is required, however, by continuing treatment, clinicians are attesting that the services billed are: 1. Qualified for the cap exception, 2. Are reasonable and necessary services that require the skills of a therapist and 3. Are justified by appropriate documentation in the medical record. The manual medical review process is required for all patients who reach $3700 in reimbursed services. The process will require that clinicians obtain advanced approval from Medicare. Criteria for medical review will be based on current medical review standards. Clinicians must comply with coverage, documentation and coding requirements set forth in the Medicare Benefit Manual (Publication 100-02, chapter 15, section 220) and the Medicare Administrative Contractor (MAC) local coverage determination (LCD) for their jurisdiction.
Patient Corner
What are the outpatient therapy limits for 2012?
- $1,880 for physical therapy (PT) and speech-language pathology (SLP) services combined
- $1,880 for occupational therapy (OT) services After you pay your yearly deductible for Medicare Part B (Medical Insurance), Medicare pays its share (80%), and you pay your share (20%) of the cost for the therapy services. The Part B deductible is $140 for 2012. Medicare will pay its share for therapy services until the total amount paid by both you and Medicare reaches either one of the therapy cap limits. Amounts paid by you may include costs like the deductible and coinsurance.
What can I do if I need services that will go above the outpatient therapy cap amounts?
- You may qualify to get an exception to the therapy cap limits so that Medicare will continue to pay its share for your therapy services. Your therapist must document your need for medically-necessary services in your medical record, and your therapist’s billing office must indicate on your claim for services above the therapy cap that your outpatient therapy services are medically necessary. Even if your therapist provides documentation that your services were medically necessary, you might still have to pay for costs above the $1,880 therapy cap limits. If Medicare finds, at any time (even after your therapy services have been paid for), that the services above the therapy cap limits weren’t medically necessary, you might have to pay for the total cost of the services above the $1,880 therapy cap limits. Starting October 1, 2012, a Medicare contractor may review your medical records to check for medical necessity if you got outpatient therapy services in 2012 higher than these amounts: $3,700 for PT and SLP combined. $3,700 for OT Note: The Medicare contractor may conduct this review of your medical records before you get any additional outpatient therapy services.
How can I find out if my therapy services will go above the therapy cap limits?
- Ask your therapist’s billing office. If you get all your therapy in the same place, your therapist’s billing office will have the most up-to-date information and will know if your services will go above these limits.
- Visit www.MyMedicare.gov to track your claims for therapy services. This website is Medicare’s secure online service for accessing your personal Medicare information.
- Check your “Medicare Summary Notice” (MSN). This is the notice you get in the mail (usually every 3 months) that lists the services you had and the amount you may be billed.
What is an ABN?
- An ABN is an Advanced Beneficiary Notification. You may be asked by your clinical provider to sign this form prior to receipt of therapy services. The form states that in the event your services are not covered under medicare, you (The patient) will become responsible for payment. It is important to ensure that the provider includes a specific monetary amount that you would be billed. You should maintain a copy of this report for your personal records
Peter Belafsky, MD, PhD, MPH

Professor and Director of Voice & Swallowing Center at UC Davis Medical Center
Dr. Belafsky’s primary clinical interests are the comprehensive diagnosis and management of voice, swallowing, and airway disorders. As Medical Director of the Voice and Swallowing Center at UC Davis, Dr. Belafsky treats a wide array of laryngeal and esophageal disorders. These disorders include but are not limited to vocal fold paralysis and paresis, vocal fold dysfunction, laryngopharyngeal reflux, chronic cough, and dysphagia caused by stroke, ALS, Zenker’s diverticulum, esophageal motility disorders, Parkinson’s disease, and swallowing problems suffered as a consequence of the treatment of head and neck cancer. Dr. Belafsky has pioneered minimally invasive treatments of voice and swallowing disorders. Minimally invasive in-office procedures performed by Dr. Belafsky at the Center include unsedated treatment of laryngeal polyps, leukoplakia, and papillomas, subglottic, tracheal, and esophageal strictures, and office-based vocal fold medialization. Dr. Belafsky’s primary research focus is the development of an artificial swallowing mechanism. He has created a medical device that can manually control the upper esophageal sphincter and is working on a comprehensive swallow propulsion system. He is also pursuing his interest in bloodless surgery through the use of radio frequency probes and non-contact lasers.
- CASE: 82 yo male presented with the chief complaint of solid food dysphagia and moderate dysphonia. He reported a 15lb weight loss over the past 18 months and 1 episode of pneumonia requiring hospitalization 5 months previous.
- PMHx: Hypertension, hypercholesterolemia, Parkinson’s disease
- PSurgHx: Inguinal hernia repair, rotator cuff repair
- ALLERGIES: None
- MEDS: Lipitor, Cardizem
- SOCIAL HISTORY: Retired Air Force Colonel, served in Vietnam War. No tobacco or illicit drug use. Social ETOH. Lives at home with his wife of 49 years. 3 children and 7 grand children. Good familial support.
- REVIEW OF SYMPTOMS: Solid food dysphagia, Hypertension, urinary frequency, weight loss, mild resting tremor, dysphonia
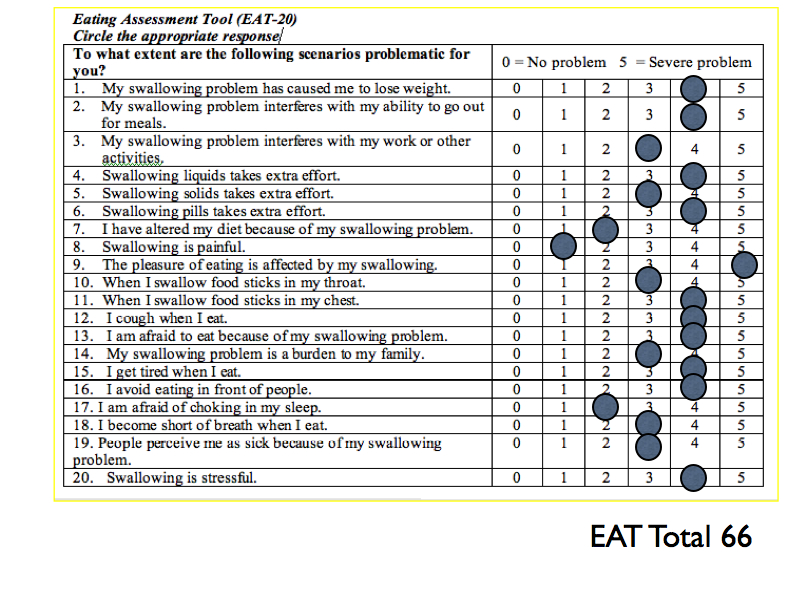
- SELF-RATINGS:
- PHYSICAL EXAM: Comprehensive head and neck examination unremarkable. Mild upper extremity resting tremor and mild bradykinesia. Oral motor examination unremarkable. Moderate breathy dysphonia.
- FEES: moderate laryngeal edema with underlying vocal fold atrophy, posterior commissure hypertrophy, mild arytenoid hyperemia. Pharyngeal strength and sensation appeared intact. There was significant post-swallow regurgitation with puree with no evidence of penetration or aspiration during the swallow.
- MBSE: Videofluoroscopic swallow study revealed evidence of a moderately obstructing cricopharyngeus muscle bar and an early Zenker Diverticulum. There was delayed pharyngeal transit time but no evidence of penetration or aspiration.
- TREATMENT RECOMMENDATIONS:
- Swallowing and voice therapy. Swallow for life program with iSwallow. EMST. LSVT. (Feel free to add to this).
- The patient was offered a cricopharyngeus muscle myotomy and a medialization laryngoplasty or an injection medialization of the vocal folds and a CP botulinum toxin injection. Because of his advanced age the patient desired an injection medialization and a CP botulinum toxin injection.
- WATCH MEDIALIZATION (0.4cc of calcium hydrozylapatite injected into each true vocal fold)
-
- WATCH BOTOX INJECTION (60 units of botulinum toxin injected into the cricopharyngeus muscle)
- OUTCOME: Post-therapy and Postoperatively the patient reported a significant improvement in voice and swallowing function. Repeat videofluoroscopy revealed improved bolus transit through the pharyngoesophageal segment with near complete resolution of the Zenker’s Diverticulum.
- FOLLOW-UP: He will be monitored closely for a progression of his dysphagia when the botulinum toxin wears off in 6-9 months. He will continue with his Swallow for Life Program.